- Scribes
- Visibility
- Speech Recognition
“This job would be great if I didn’t have to chart.” Physicians say this all the time. One way to not have to chart (much) is to work with a Federal Disaster Medical Assistance Team (DMAT) team. Although the National Disaster Medical System now has an electronic medical record (EMR) system, it used to just use scribbling on paper charts. And, since you have sovereign immunity against lawsuits, and you aren’t using your charts for billing, charting could be quite minimal. I have personal knowledge of a medical team in the field, after Hurricane Katrina, in a small, isolated town for a several-hour medical clinic; the team used 8.5×11″ paper on a clipboard for charting, and each patient got one line.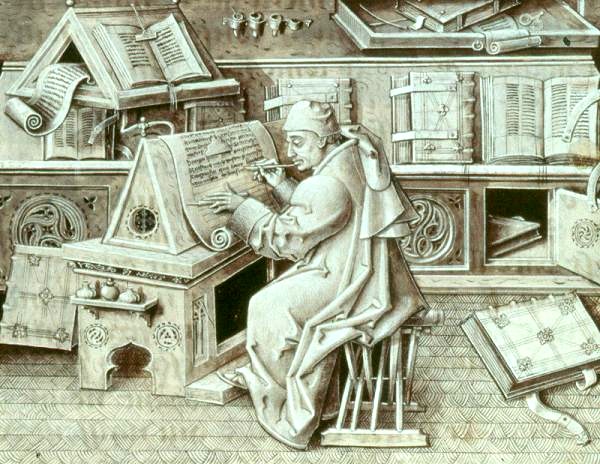
This isn’t feasible for most real-life physician medical charting. We do have to use our charts for billing, and for protection against lawsuits. (“If you didn’t chart it, it wasn’t done.”)
We also are sometimes faced with the demand for charting so that, instead of a narrative string of ASCII text, our charts are a small database of discrete, labeled elements (e.g., Chief Complaint: chest pain. Duration: 1 day.) This latter is known as structured charting, and is eagerly promoted by researchers, who want structured data, and billing companies, who enjoy the resulting ease of assuring compliance with billing and coding rules.
Some template systems are easy and fast for physicians to use, such as the famed and very-profitable paper T-sheets from T-system (there are also many reputable competitors). They are also great for billing, but hard to defend in court. They are easy enough to use that, if you’re using them, you really don’t need scribes. There are electronic versions of the T-sheets and competitors, and on a tablet such as an iPad, they are very attractive – but still not as easy as paper templates.
T-sheets and the like are, in a sense, structured charting, but the data elements are hard to capture from a scanned chart, so researchers and those involved in QI activities aren’t as enamored of them. They want electronic structured data. So the rest of this post will be devoted to electronic structured charting.
If you’re dictating into a phone, dictating takes quite a while, and I know places that use such dictation who are thinking about scribes. But instead of having the scribes dictate into a phone, the scribes would use an electronic structured charting application to complete the chart. There also are places that use speech-recognition for charting – in fact I’ve been doing ED charting via speech-recognition for over ten years – which has advantages over dictating into a telephone. For example, you can dictate the History of Present Illness (HPI) on each patient right after you see them, even if you’re pretty busy. Later, when you have a chance to complete the chart, you can see that HPI that you dictated, which really helps you remember the patient and do a more accurate chart. However, this produces a string of ASCII text rather than electronic structured data.
I’ve tried using point-and-click charting, with speech-recognition to fill in the HPI and medical decision-making sections. Switching modes from point-and-click back and forth to dictation is awkward and slowed me down. It seemed a lot slower than simply using speech-recognition to do the whole chart.
There are other advantages to electronic structured charting; it’s easy to put in reminders to chart important things (e.g., neck and fontanelle exams for kids with fever). Electronic charting systems may also be integrated with computer-based practitioner order entry (CPOE) and other systems, allowing interaction checking between existing medications and prescribed or ordered medications (which has its own set of pros and cons to discuss), and providing easy look-up of appropriate reference information. Electronic structured charting (at least if you do a good job of haggling with the vendor before signing the contract) is a lot cheaper than traditional dictation-into-a-telephone. Which, by the way, uses speech-recognition as a front-end; rather than true transcriptionists, the people who review the output of the first-stage speech-recognition are better termed correctionists.
But, as many emergency physician informatics doyens such as Todd Taylor and Rick Bukata maintain, using a highly-paid physician to to a data-entry clerk’s job just doesn’t make economic sense. Except that electronic structured charting (Unless you’re a hospital administrator and you don’t care about the impact on the pay and satisfaction of your emergency physicians to cut your bottom line for transcription costs.) But the pressure from researchers, coders and administrators is hard to resist.
Thus, scribes.
Scribes are now well-established in many community EDs, and used in a few academic settings. Community EDs tend to contract with a company that trains, vets and provides scribes, whereas academic EDs, which tend to be in college towns, generally set up their own program to train and vet scribes.
The Emergency Medicine Practice Committee of the American College of Emergency Physicians has prepared a detailed white paper on the subject of scribes that provides much more information about scribe programs. But I hope that the above adds somewhat, though perhaps a bit opinionated, to what the white paper provides.
Tags: ED Systems, Emergency Department, ED, Charting, Healthcare, IT, Healthcare IT, Scribes

