Meaningful Use has become a less-meaningful phrase in the USA over the past year or so, at least to those of us who work in the ED. Intentionally or no, politicians twist and deform the English language like no others. Their latest target, at least as far as Emergency Department computer systems are concerned, is the phrase: meaningful use.
In this post, I will grossly oversimplify to help provide a basic understanding of what meaning ful use now seems to mean and why you should care. As Bacon observed: we are more likely to reach the truth through error than through confusion.
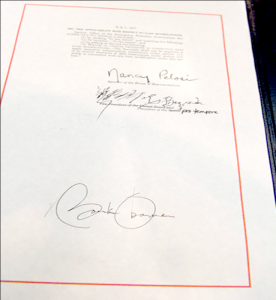
The American Recovery and Reinvestment Act of 2009 (ARRA) contains a vast wealth of provisions to reinvigorate the US economy (no pun intended). Of interest to readers of this site is that the ARRA says that, if you show new meaningful use of electronic medical records, then you can get money from the Federal government. However, this meaningful use only applies to office-based physicians and hospitals, so emergency physicians and Emergency Departments, by themselves, can’t get any money. However, in order for hospitals to get the money, the ED and the emergency physicians have to cooperate – which means you have some power over the administration. (Not too much, though – if you’re too uncooperative they can fire you or terminate your contract. Don’t laugh. It has happened.)
Here are ARRA Objectives for meaningful use (by hospitals; the objectives for office-based physicians are different).
- Objective: Use of CPOE for orders (any type) directly entered by authorizing provider (for example, MD, DO, RN, PA, NP).
Measure: CPOE is used for at least 10 percent of all orders. - Objective: Implement drug-drug, drug-allergy, drug- formulary checks.
Measure: The eligible hospital has enabled this functionality. - Objective: Maintain an up-to-date problem list of current and active diagnoses based on ICD-9-CM or SNOMED CT.
Measure: At least 80 percent of all unique patients admitted to the eligible hospital have at least one entry or an indication of none recorded as structured data. - Hospital Objective: Maintain active medication list.
Measure: At least 80 percent of all unique patients admitted by the eligible hospital have at least one entry (or an indication of “none” if the patient is not currently prescribed any medication) recorded as structured data. - Objective: Maintain active medication allergy list.
Measure: At least 80 percent of all unique patients admitted to the eligible hospital have at least one entry (or an indication of “none” if the patient has no medication allergies) recorded as structured data. - Objective: Record demographics.
Measure: At least 80 percent of all unique patients admitted to the eligible hospital have demographics recorded as structured data. - Objective: Record and chart changes in vital signs.
Measure: For at least 80 percent of all unique patients age 2 and over admitted to the eligible hospital, record blood pressure and BMI; additionally, plot growth chart for children age 2 to 20. - Objective: Record smoking status for patients 13 years old or older.
Measure: At least 80 percent of all unique patients 13 years old or older admitted to the eligible hospital have “smoking status” recorded. - Objective: Incorporate clinical lab-test results into EHR as structured data.
Measure: At least 50 percent of all clinical lab tests results ordered by an authorized provider of the eligible hospital during the EHR reporting period whose results are in either in a positive/negative or numerical format are incorporated in certified EHR technology as structured data. - Objective: Generate lists of patients by specific conditions to use for quality improvement, reduction of disparities, research, and outreach.
Measure: Generate at least one report listing patients of the eligible hospital with a specific condition. - Objective: Report hospital quality measures to CMS or the States.
Measure: For 2011, an eligible hospital would provide the aggregate numerator and denominator through attestation as discussed in section II.A.3 of this proposed rule. For 2012, an eligible hospital would electronically submit the measures are discussed in section II.A.3. of this proposed rule. - Objective: Implement five clinical decision support rules relevant to specialty or high clinical priority, including for diagnostic test ordering, along with the ability to track compliance with those rules.
Measure: Implement five clinical decision support rules relevant to the clinical quality metrics the Eligible Hospital is responsible for as described further in section II.A.3.
Having browsed through this list, you might come to a few conclusions, such as:
- Most of this has little to do with the ED.
- Given how much of the volume of the hospital passes through the ED, if your hospital is going after ARRA funds, the administration may demand that your nurses or physicians are obsessive and compulsive about gathering information on smoking (no big deal) and growth information on all pediatric admissions(a bigger deal, because it basically has no relevance to the emergency management of a pediatric patient, and is seldom routinely obtained on ED patients).
But the big one is likely CPOE. What percentage of your hospital’s admissions come through the ED? More than 50%? Maybe more like 70%? What percentage of your hospital’s outpatient volume comes through the ED? If CPOE is going to be used for 10% of all orders, that likely means that at least some of the patients in the ED will need to use CPOE, which means that the ED will have to use CPOE. (There are some fallacies with this argument, but it will probably hold, nonetheless, especially as the percentage increases as the years roll on and the criteria for additional $$ are tightened.)
Your hospital’s systems have to meet the above meaningful use requirements. But they will have to be certified by a certifying agency approved by the government. Originally, it was only going to be CCHITT that was allowed to certify systems. But after vendor complaints of monopoly (perhaps the $35,000 cost for certification contributed to this), two others were added, for a total of three:
- Certification Commission for Health Information Technology (CCHIT) – Chicago, Ill. Date of authorization: September 3, 2010.
- Drummond Group, Inc. (DGI) – Austin, Texas. Date of authorization: September 3, 2010.
- InfoGard Laboratories, Inc. – San Luis Obispo, CA Date of authorization: September 24, 2010.
So that’s the skinny on meaningful use. Until next year, when they will revise the criteria. Look for a higher percentage of CPOE (=EDs will all have to do CPOE if you want the $$) and other new requirements.
Addendum January 2011:
Lawrence Wenzlow’s Rural Health IT blog has a nice entry on the (now) two different ways that ED patients may be counted for the “denominator” for the above calculations: admitted/obs or all patients. Another post there discusses recent events in this rapidly-changing field, such as the Feds allowing nurses or secretaries to enter order for doctors and still consider it “CPOE” for the purposes of ARRA. There is a page at the Physician’s EHR site that provides a quick summary of the Final Rule. And remember, when all this seems hopelessly confusing, go back to the appropriate pages of the Federal Register (July 28,2010) which show the complete Final Rule text of the ARRA Healthcare IT Stage 1 regulations.
Tags: ARRA, Computers, ED, ED Systems, Healthcare, Healthcare IT, IT, Meaningful Use