Many people use the terms electronic medical record (EMR), electronic health record (EHR) and personal health record (PHR) interchangeably. But arguably they mean very different things.
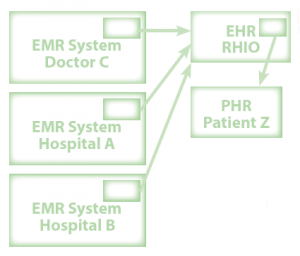
There are also a great variety of other terms used to describe electronic records, but EMR and EHR and PHR are now more-or-less accepted as the three real terms. In fact, the US ONCHIT commissioned the NAHIT (an organization that lasted a grand total of seven (7) years) to develop definitions and so, at least in the USA, these are official. You might want to refer to the schematic below and to the right.
An EMR is just that – an electronic record of an episode of medical care, whether inpatient or outpatient or ED. The EHR is both more and less than the EMR – it is those parts of the EMR that are appropriately shared with stakeholders outside the hospital, doctor‘s office or other EMR source. Parts of the EMR are shared, as the EHR insurance companies, government agencies, patients themselves, and employers. An article in Medical Economics, quoting an Institute of Medicine report, defines the elements of an EHR thusly:
- Health information and data. The system holds what‘s normally in a paper chart – problem lists, medication lists, test results.
- Results management. An EHR lets you receive lab results, radiology reports, and even X-ray images electronically.
- Order entry. No more prescription pads. All your orders are automated.
- Decision support. An EHR is smart enough to warn you about drug interactions, help you make a diagnosis, and point you to evidence-based guidelines when you ponder treatment options.
- Electronic communications and connectivity. You can talk in cyberspace with patients, your medical assistant, referring doctors, hospitals, and insurers—securely. And your system interfaces with everyone else‘s. Interoperability is the key word.
- Patient support. Patients can receive educational material via the EHR and enter data themselves through online questionnaires and home monitoring devices.
- Administrative processes. The system lends a hand with practice management. Patients can schedule their own appointments and staffers can check on insurance eligibility.
- Reporting and population health management. How many patients did you treat for tuberculosis in 2003? How many of your diabetics have their HbA1c under 7? An EHR will spit out the answers, thanks to a searchable database.
A Personal Health Record is just that: personal. It is those parts of the EMR/EHR that an individual person “owns” and controls. Google and Microsoft want to help you with this. (Really. And if these definitions seem a bit vague, well, yes, they are, because we’re just getting started with this stuff, you know?)
The NAHIT report defines the following:
Electronic Medical Record (EMR): An electronic record of health-related information on an individual that can be created, gathered, managed, and consulted by authorized clinicians and staff within one health care organization.
Electronic Health Record (EHR): An electronic record of health-related information on an individual that conforms to nationally recognized interoperability standards and that can be created, managed, and consulted by authorized clinicians and staff across more than one health care organization.
Personal Health Record (PHR): An electronic record of health-related information on an individual that conforms to nationally recognized interoperability standards and that can be drawn from multiple sources while being managed, shared, and controlled by the individual.
Regional Health Information Organization (RHIO): A health information organization that brings together health care stakeholders within a defined geographic area and governs health information exchange among them for the purpose of improving health and care in that community.
EMR adoption by hospitals, which is a prerequisite for EHRs and PHRs is rated on a 0-7 scale, with 0 being no EMR and 7 being a full, totally paperless EMR. On this scale, in 2007, about 20% of hospitals were at Stage 0, 20% at Stage 1, 50% at Stage 2, and 10% at Stage 3. None were at Stage 7, but as of December 2009, 28 hospitals (less than 1%) had reached Stage 7 (HIMSS data).